September 12, 2022
Nearly 50 million individuals receive prescription drug coverage through a Medicare Part D plan. As with other Medicare options, Part D plans range in cost and coverage. This means choosing the plan that best fits your unique needs may be difficult but is incredibly important. When determining which plan to enroll in, beneficiaries should not only consider what coverage the plan provides but also where any gaps in coverage may lie. One such common coverage gap is known as the “donut hole.”
The Medicare Part D donut hole refers to the stage when Medicare beneficiaries have met certain out-of-pocket thresholds and therefore must pay a larger portion of their prescription drug costs, until they reach the catastrophic coverage level. Originally the cost-share requirements in the donut hole were much higher, with instances of beneficiaries paying 100% of prescription drug costs once they reached this stage. Changes have been made in recent years, and now, while in the donut hole, beneficiaries will be responsible for up to 25% of prescription costs. It is important for Medicare beneficiaries to understand the various stages of Part D coverage, including the donut hole, so they can be prepared as their out-of-pocket expenses fluctuate throughout the year.
Stages of Part D prescription drug coverage
Medicare Part D plans typically have four stages of coverage for prescription drugs. These plans will last from January 1st through December 31st, and will reset the following calendar year:
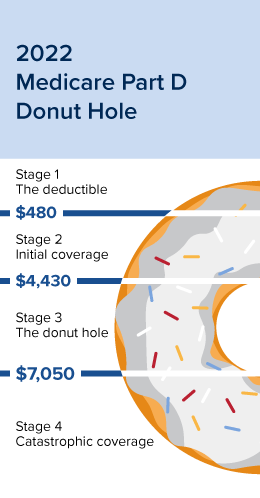 Stage 1 – The deductible: At this stage, beneficiaries are required to pay 100% of prescription costs until the deductible is met before the drug plan will begin to cover its share. Deductibles will vary among plans, but each year the Centers for Medicare and Medicaid Services (CMS) establish a cap that cannot be exceeded. For 2022, the deductible cannot exceed $480.
Stage 1 – The deductible: At this stage, beneficiaries are required to pay 100% of prescription costs until the deductible is met before the drug plan will begin to cover its share. Deductibles will vary among plans, but each year the Centers for Medicare and Medicaid Services (CMS) establish a cap that cannot be exceeded. For 2022, the deductible cannot exceed $480.
Stage 2 – Initial coverage: After the deductible has been met, the drug plan will begin to cover its share. If the plan utilizes copays, the beneficiary may expect to pay a standard amount per drug based upon the tier the prescription falls into. For beneficiaries with coinsurance, the amount they pay may vary throughout the year depending on the cost of the drug. Once the beneficiary and the plan have paid the CMS established maximum, the beneficiary will move into the donut hole. In 2022, the maximum is $4,430, which includes the deductible.
Stage 3 – The coverage gap (or, the donut hole): Once beneficiaries reach this stage, a temporary limit is placed on what the drug plan will pay for covered prescriptions. Once in the gap, beneficiaries pay no more than 25% of the cost of brand-name and generic prescription drugs covered by the drug plan, with the plan paying the rest. In addition, the beneficiary is required to pay 25% of the dispensing fee associated with brand-name drugs. Beneficiaries will remain within the donut hole until the CMS-designated out-of-pocket cost is met. For 2022, this limit is $7,050 and includes the deductible, coinsurance, copayments, and the cost of covered prescriptions, not including any dispensing fees.
Stage 4 – Catastrophic coverage: After the out-of-pocket-cost threshold is met, beneficiaries move to the catastrophic coverage stage. At this stage, beneficiaries will only typically pay about 5% coinsurance or a small copay amount for any prescriptions for the remainder of the year. Once at this stage, beneficiaries will remain here until the next calendar year.
Is it possible to avoid the donut hole?
The donut hole only applies to those beneficiaries who utilize Part D for prescription drug coverage. Even still, not everyone will fall into the donut hole. For those who are concerned about costs associated with coverage, there are options to help avoid the donut hole.
-
- Compare prescription drug plans each year: As with most healthcare and medical coverage, prescription drug plans can change from year to year. It is important that beneficiaries review coverage each year to determine if their plan still provides the best possible coverage for their individual needs.
- Utilize generics over-brand name drugs: In many instances, generic prescriptions will be available at significant cost savings. If there is an available option and the beneficiary’s medical provider is comfortable with a generic drug instead of a name-brand drug, choosing those may be more cost-effective.
- Look into Extra Help: Medicare’s Extra Help program is designed to help beneficiaries with limited income and resources pay for premiums, deductibles, coinsurance, copays, and other costs. Those who qualify for the Extra Help program will not enter the donut hole.
Stay ahead and stay prepared
Medicare’s Annual Election Period (AEP) runs each year from October 15th through December 7th. During this time, beneficiaries who wish to add, change, or disenroll in a Part D prescription drug coverage plan will have the chance to do so. If you have fallen into the donut hole or are concerned about doing so, now may be the time to review the options available ahead of AEP.
Contact Aevo Insurance Services, a division of Brown & Brown Absence Services Group, to speak with an experienced licensed insurance agent about your Medicare options, including those for Part D plans. Our guidance extends through every step of the enrollment process, starting with helping select a Medicare plan that meets your unique medical and financial needs.
Please note that as of 2021, The Advocator Group now conducts business as Brown & Brown Absence Services Group. While our name may have changed, our commitment to excellent service and helping our clients in as many ways as possible has not.
We do not offer every plan available in your area. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1-800-MEDICARE to get information on all your options.